Do you worry your baby isn’t getting enough to eat? You aren’t alone. It is the number one concern for new moms.
I remember the panic of pumping and seeing barely an ounce, wondering if my body was failing my baby. But here is the truth: low supply is often a misunderstanding of how breastfeeding works. And even if your supply is truly low, you can fix it.
I found solutions to boost my output without losing my mind. Here is how you can too.
Is Your Milk Supply Really Low?
Before you panic-buy lactation cookies or pump until you are sore, you need to determine if your supply is actually low. It is common to confuse normal breastfeeding behavior with a lack of milk.
However, true low supply does exist. It can stem from management issues or underlying medical conditions. If you suspect a medical issue, consult a lactation professional immediately.
Here is how to tell the difference between a dip in supply and false alarms.
How Much Milk Should You Be Producing?
If your milk ducts are playing hooky, your baby will show specific signs. Forget the pump output for a second; look at the baby.
Do You Really Have a Low Supply or Do You Have False Expectations?
Many women believe they have low supply because they don’t feel “full” or their baby acts hungry. often, these are normal developmental stages.
It is frustrating to pump for 20 minutes and get less than 2 ounces, but that can be a normal amount depending on your baby’s age and nursing habits.
Here are common “false alarms” that trick moms into worrying.
Is A Medical Condition Affecting Supply?
If the signs point to true low supply, check your medical history. Certain conditions can inhibit production.
When to Blame It on the Baby?
Sometimes the factory is fine, but the customer is having trouble picking up the order.
Tips for Increasing Milk Supply

1. Take it Easy Momma
Stress is a supply killer because it inhibits oxytocin, the hormone responsible for “let-down.” You can’t make milk flow if you are tense.
Ask your partner or family to handle diapers and laundry while you focus solely on feeding and resting.
- Practice deep breathing or visualization before nursing.
- Get fresh air; a 10-minute walk can reset your mood.
- Sleep when you can. I know, “sleep when the baby sleeps” is annoying advice, but rest is crucial for recovery and production.
I struggled to ask for help with my firstborn. Once I finally let my husband take the night shift for soothing (bringing the baby to me only to feed), my sleep improved, and so did my supply.
2. Take In Plenty of Fluids
You can’t pour from an empty cup. Breast milk is mostly water, so stay hydrated. You don’t need to drown yourself, but aim to drink to thirst and then a little more (9).
Keep a water bottle at your nursing station. If your urine is dark yellow, drink more. Electrolyte drinks are helpful but watch the sugar content.
Watch Out For
3. Watch Your Food Selections Carefully
Foods That Increase Milk Supply
- Fruits and vegetables: Carrots, leafy greens, and garlic.
- Healthy Fats: Avocados, nuts, and flaxseed.
- Whole Grains: Oats and barley are famous for boosting supply.
- Protein: Eggs, lean meats, and legumes.
While you should eat well, don’t stress about a perfect diet. You can make milk on a diet of toast and tea, but you will feel better if you eat nutrient-dense foods.
4. Be Careful When Messing with Your Hormones
Hormones run the show. If your period returns, you might see a temporary dip in supply during ovulation or menstruation. Calcium and magnesium supplements can help mitigate this drop.
Be wary of birth control. If you must use hormonal contraception, insist on progestin-only options (mini-pill or IUDs) to protect your supply.
5. Only Take Medications If They’re Necessary
Certain cold and allergy meds, specifically pseudoephedrine (Sudafed), dry up secretions, including breast milk. Antihistamines can have a similar effect.
Take Note
6. Make Sure You’re Getting Enough to Eat
Now is not the time for a crash diet. Breastfeeding burns about 500 calories a day. To keep the factory running, you need to eat at least 2,000 to 2,500 calories daily (12).
If you are hungry, eat. Your body is doing hard work. Keep easy snacks like trail mix, yogurt, or bananas handy for one-handed eating while nursing.
7. Don’t Rely on Supplements Alone
Fenugreek, Blessed Thistle, and lactation cookies can help, but they are not magic bullets. They work best when combined with frequent milk removal.
Note that some herbs can decrease supply. Avoid large amounts of peppermint, sage, parsley, and oregano (13). Culinary amounts in food are fine, but avoid concentrated oils or teas of these herbs.

Nursing Tips To Produce More Milk

Breast milk production is a supply and demand system. The more milk you remove, the more your body makes. Here is how to maximize that signal.
8. Avoid Formula Supplementation or Bottles
Every bottle of formula your baby drinks is a missed signal to your body to produce that milk. If possible, avoid supplementing unless medically necessary.
Remember
If you must supplement, use a slow-flow nipple and “paced feeding” techniques to mimic the effort of breastfeeding. Mimijumi bottles are often recommended for breastfed babies.
9. Tinker With Your Baby’s Latch
A good latch is critical. Your baby needs to take a large mouthful of breast tissue, not just the nipple.
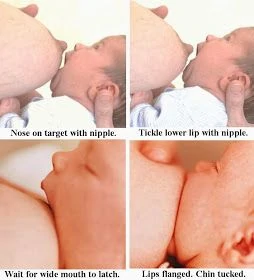
Look for “fish lips” (flanged outward). If nursing hurts, break the suction gently with your finger and try again. Pain is a sign something is wrong.
10. Get Comfy
If you are hunched over and tense, milk flow suffers. Use a nursing pillow to bring the baby up to breast height so you aren’t leaning forward.
Experiment with positions like the Football Hold (great for C-sections or large breasts) or the Cross-Cradle hold for better control.
11. Don’t Be Afraid to Have a Hands-On Experience
Hands-on pumping or nursing involves massaging and compressing your breast while the baby feeds or the pump runs. This helps empty the breast more thoroughly, which increases the fat content of the milk and signals your body to make more.
12. Give Switch Nursing and Double Nursing a Whirl
Switch nursing: If your baby gets sleepy or flow slows down, switch them to the other breast. Keep switching back and forth (ping-ponging) during one feed to keep them active.
Double nursing: Nurse the baby, take a 10-15 minute break to burp or change a diaper, and then put them back on the breast. This mimics cluster feeding.
13. Nurse More Frequently
Forget the clock. Nurse on demand. If you are trying to boost supply, aim for a minimum of 8-12 feedings every 24 hours.
Top Tip
14. Keep Your Eyes on Your Baby
Sensory input matters. Smelling your baby’s head and looking at them releases oxytocin. If you are pumping at work, look at videos or photos of your baby to help trigger a let-down.
15. Keep Nursing at Night
Prolactin levels (the milk-making hormone) are highest at night. Night feedings are crucial for establishing and maintaining supply. I know it is exhausting, but those 3 a.m. sessions are doing the heavy lifting for your supply.
Because prolactin (the milk-making hormone) levels are higher at night, nursing or pumping at night, even once a night, will increase your supply. If you’re skipping pumping sessions, you’re missing out on your full potential.
Editor's Note:
Michelle Roth, BA, IBCLC16. Use the Skin to Skin Method
Strip your baby down to a diaper and place them against your bare chest. This “kangaroo care” regulates the baby’s heart rate and triggers your feeding hormones. It is a powerful reset button for nursing strikes or supply dips (14).
17. Use Pacifiers Sparingly
In the early weeks, every suck should ideally be at the breast. Pacifiers can mask hunger cues, causing you to miss a feeding session. Wait until breastfeeding is well-established (around 4 weeks) before introducing a dummy (15).
18. Keep Your Baby Awake While Breastfeeding
A sleeping baby doesn’t eat. To keep them active:
- Tickle their feet or stroke their cheek.
- Blow gently on their face.
- Change their diaper between breasts.
- Do breast compressions to shoot a fast stream of milk that wakes them up.
19. Throw Out the Nipple Shields
Nipple shields are tools, not lifestyle choices. While they can save a breastfeeding relationship in specific cases, they can also reduce milk transfer stimulation (16). Work with a lactation consultant to wean off the shield as soon as possible.
20. Increase Your Supply With Pumping
Adding pump sessions is a classic way to boost supply.
- Pump after nursing: Pump for 10-15 minutes after the baby eats to ensure the breast is fully empty.
- Pump between feeds: Add a session an hour after nursing.
Don’t worry if you don’t see much output. The goal isn’t just the milk in the bottle; it is the stimulation that tells your body “make more tomorrow.”
21. Use Power Pumping To Increase Your Supply
Power pumping mimics a baby cluster feeding. It is intense but effective.
How Power Pumping Works
- Pump 20 minutes. Rest 10 minutes.
- Pump 10 minutes. Rest 10 minutes.
- Pump 10 minutes. Finish.
Do this for 3-4 days in a row to see results (17).
Taking Care of Your Breasts

Healthy breasts make more milk. Ignore pain or lumps at your own peril.
22. Don’t Forget to Massage Them
Massage stimulates blood flow and helps move fat-rich hindmilk forward. Massage before and during pumping to maximize output. It also helps prevent clogged ducts.
23. Use Breast Compressions
Breast compression is essentially squeezing the breast like a tube of toothpaste to help the baby get more milk.
24. Heat Things Up
Warmth dilates ducts and encourages flow.
- Take a hot shower before nursing.
- Use warm compresses or heating pads (specifically designed for breasts) right before you pump.
- Massage under warm water.
25. Try to Avoid Engorgement
Engorgement signals your body that it made too much milk, triggering a reduction in supply. It also puts you at risk for mastitis. If you cannot nurse, pump or hand express just enough to relieve the pressure.
Prolonged engorgement can also lead to low supply – full breasts release a chemical signal that tells your breasts not so much milk is needed.
Editor's Note:
Michelle Roth, BA, IBCLCFAQs
Putting It All Together
Struggling with supply is exhausting, but it is rarely permanent. I noticed a big improvement in just one week by focusing on hydration, rest, and frequent nursing.
Don’t try to do all 25 tips at once. Pick three that resonate with you, maybe the skin-to-skin contact, the water intake, and the breast compressions, and start there. You can handle this.