You’re ready to hang up the flanges. Whether you’re returning to work, your baby is weaning, or you’re just done, stopping breast pumping is a major milestone. But quitting cold turkey is a recipe for clogged ducts and painful infections.
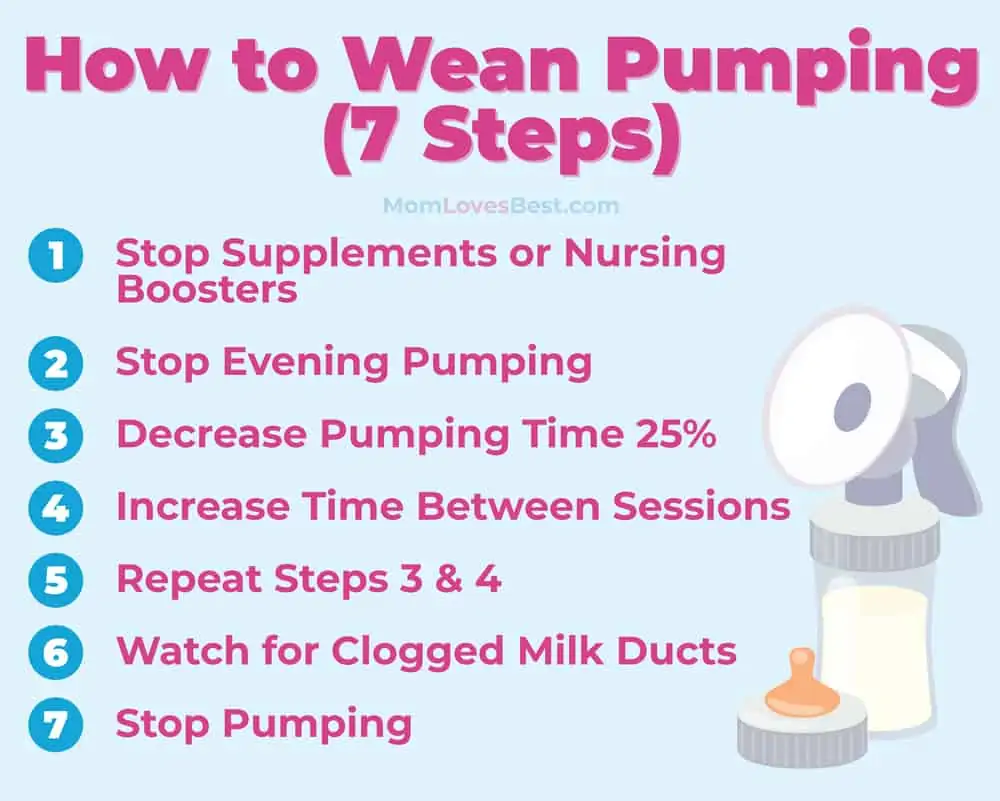
We’ve combined medical research with real-world experience to create a safe, seven-step exit strategy. Here is everything you need to know to wean from the pump without the agony.
Key Takeaways
Quitting abruptly can lead to mastitis, so the golden rule is “slow and steady.” To safely wean from the breast pump:
- Stop Boosters: Immediately cut out galactagogues like fenugreek or lactation cookies.
- Target Evenings First: Drop your late-day sessions first since prolactin levels are naturally lower then.
- Shrink the Time: Shave 2–5 minutes off each session until you are just “comfort pumping.”
- Space It Out: Gradually extend the gap between pumps until you can skip them entirely without pain.
How Do I Wean From the Pump?
When a baby weans from the breast naturally, they slowly drink less over time. Your body gets the signal that demand is down, so it lowers the supply. It’s a seamless biological feedback loop.
Weaning from a breast pump requires you to manually replicate that process. You have to trick your body into thinking the “baby” isn’t hungry anymore.
There are a few ways to tackle this:
- Drop Sessions: Completely removing one pump per day every few days.
- Shrink Sessions: Pumping for less time during every session.
- Stretch Intervals: Going longer between pumps (e.g., every 5 hours instead of 4).
- Cold Turkey: Stopping abruptly (Not recommended).
Keep In Mind
Thankfully, it is easier to stop milk production than it is to start it. If you follow the steps below, you can dry up your supply with minimal drama.
How to Stop Pumping Breast Milk in 7 Steps
Here is the safest roadmap to retire your pump.
1. Stop Supplements and Nursing Boosters
If you are eating oatmeal, drinking nursing tea, or popping fenugreek to keep your output high, stop immediately. Your goal now is to reduce supply, not protect it. If you are on prescription medication like Domperidone, ask your doctor for a tapering schedule.
2. Drop Evening Pumping Sessions
Your milk-making hormone, prolactin, naturally peaks in the early morning and drops in the evening (2).
Start by dropping the pump session right before bed or in the late afternoon. Since your supply is naturally lower at this time, your breasts are less likely to become engorged, making this the easiest session to eliminate.
3. Decrease Pumping Time by 25%
Start cutting your pump time to signal “lower demand” to your body. If you usually pump for 20 minutes, stop at 15.
The goal here is comfort pumping. You want to remove just enough milk to relieve pressure and avoid pain, but do not empty the breast completely. Leaving some milk behind releases a protein called FIL (Feedback Inhibitor of Lactation) that tells your body to slow down production.
Maintain this shorter duration for 3–4 days before shortening it again.
4. Increase the Time Between Sessions
Stretch the gap between pumps. If you usually pump every three hours, try pushing it to four.
Listen to your body. If you feel rock hard at 3.5 hours, do a quick 5-minute pump to relieve the pressure, then stop. Do not wait until you are in extreme pain, as that invites infection. Combine this with Step 3 (shorter sessions spaced further apart) for the best results.
5. Repeat Steps 3 and 4
Rinse and repeat. Every few days, drop another session, shorten the remaining ones, or push the time back further.
6. Watch for Clogged Milk Ducts and Mastitis
You need to be vigilant during this process. A clogged duct feels like a tender lump or a “bruised” spot on the breast.
If you find a lump, pause your weaning plan. You must clear the clog before you continue dropping sessions.
- Ice and NSAIDs: Modern protocol suggests ice (to reduce inflammation) and Ibuprofen rather than aggressive heat.
- Gentle Movement: Lightly brush the skin away from the nipple (lymphatic drainage) rather than deep tissue massage, which can bruise the tissue.
- Keep Pumping: Do not stop pumping on the affected side until the clog clears.
If you develop a fever, chills, body aches, or red streaking on the breast, you likely have mastitis (3). Call your doctor immediately.
Mastitis moves fast. If you feel “flu-like” symptoms coming on, rest, hydrate, and apply cold compresses. If you don’t feel better within 24 hours, you may need antibiotics.
Editor's Note:
Michelle Roth, BA, IBCLC7. Stop Pumping
Eventually, you will be down to one short session a day, producing barely an ounce. This is the finish line.
Skip the pump and see what happens. If you feel fine after 24 hours, you are done. If you feel uncomfortable fullness, hand express just enough to get comfortable in the shower, but don’t hook up to the machine.
3 Tips to Dry Up Milk Faster
If you want to speed up the process naturally, try these tricks used by moms for generations:
1. Cabbage Leaves
It sounds like an old wives’ tale, but cold green cabbage leaves can help reduce engorgement and suppress supply. Wash the leaves, crush the veins slightly to release the enzymes, and wear them inside your bra until they wilt.
2. “No More Milk” Tea
Look for teas containing sage or peppermint. While delicious, these herbs are known generally as anti-galactagogues, meaning they help decrease milk production when consumed in large amounts.
3. Decongestants
Pseudoephedrine (found in Sudafed) is known to reduce milk supply significantly. Many moms take a dose to help dry up the final ounces. Always check with your doctor before taking new medication.
FAQs
The Bottom Line
Weaning from the pump is a journey, not a sprint. By respecting your body’s limits and reducing sessions gradually, you can avoid the pain of engorgement and the risk of mastitis.
Listen to your body, treat any clogs immediately, and give yourself grace during the hormonal shifts. You’ve put in the work—now enjoy your freedom.